
Intermittent exotropia is the outward drift of one or both eyes. It affects 1% of people. The resting position of our eyes is out. All of us are using muscle tone at all times to hold our eyes straight. If a person is given anesthesia, as they go to sleep and relax their muscle tone, the eyes spontaneously drift out. We do not know why some people allow this muscle tone to relax and for the eye to drift. However, it tends to happen most when they are sleepy, sick, or daydreaming. There are three proven ways to treat this condition. When a child needs eyeglasses, simply by putting them in the correct prescription, the eye alignment can improve. When one eye drifts more than the other, we use patch therapy to cover the good eye and force the weaker eye to work by itself. Lastly, patients with large and constant deviations sometimes require surgery. Dr. Morrison was vice-Chair of the Pediatric Eye Disease Investigator Network and has participated in many clinical trials on this condition.
Morrison D, McSwain W, Donahue S. Comparison of sensory outcomes in patients with monofixation vs. bifoveal fusion after surgery for intermittent exotropia. J AAPOS 2010; 14:47-51.ƒ
Three and Four Horizontal Muscle Surgery for Large Angle Exotropia. Chen JH, Morrison DG, Donahue SP. J Pediatr Ophthalmol Strabismus. 2015 Sep-Oct;52(5):305-10. doi: 10.3928/01913913-20150609-02. Epub 2015 Jun 15.
Summers AI, Morrison DG, Chandler DL, Henderson RJ, Chen AM, Leske DA, Walker KR, Li Z, Melia BM, Bitner DP, Kurup SD, Allen M, Phillips PH, Nash DL, Grigorian AP, Kraus CL, Miller AM, Titelbaum JR, Kraker RT, Holmes JM, Cotter SA; on behalf of PEDIG. A Pilot Randomized Clinical Trial of Relieving Base-in Prism Spectacle Treatment for Intermittent Exotropia. Optom Vis Sci 2023;100(7):432-443.
Infantile esotropia is large-angle eye crossing that starts before 6 months of age. It is generally treated with an eye muscle surgery, weakening the inside pulling muscles. This is an outpatient surgery that takes about 45 minutes to complete. A small incision is made on the white part of the eye to access the muscle. The muscle is physically moved backwards on the eye to make it weaker. There are no patches or bandages after surgery, although the eye is red at the incision site. While highly successful, many children require a second surgery with this condition at some point in their lives. Older children may also develop esotropia. Dr. Morrison will work with you to accurately diagnose your problem and provide the best treatment. In some cases, an MRI may be needed (see Sixth nerve palsy).
Morrison DG, Schnall B, Young MO. When to treat congenital esotropia. J Pediatr Ophthalmol Strabismus 2010;47:262-6.
Morrison D, Emanuel M, Donahue S. Surgical management of residual or recurrent esotropia following maximal bilateral medial rectus recession. Arch Ophthalmol. 2011;129:173-5.
Management of high AC/A ratio esotropia. Morrison DG, Olitsky SE, Raab EL. J Pediatr Ophthalmol Strabismus. 2012 Sep-Oct;49(5):265-8. doi: 10.3928/01913913-20120621-01.

Accommodative esotropia is eye crossing associated with a high need for farsighted eyeglasses. Focusing with the lens inside the eye is linked to convergence, or moving the eyes closer together. If a child has a very high need for eyeglasses in the hyperopic or farsighted direction, they can focus really hard with the lens inside the eye and still see relatively clearly. However, the constant strain of focusing eventually breaks the normal mechanism down and allows the eyes to cross. The average age of onset for this condition is between two and four years. It can be very frightening to parents as the eyes can cross quite suddenly. Proper diagnosis of this condition requires dilation of the eyes to obtain the most accurate prescription for glasses. If a child is not dilated, and the full prescription is not given, surgery may be recommended when it could have been avoided. There are some children who still have eye crossing even with the best glasses. In those children, both glasses and surgery are necessary.

The 6th cranial nerve, or abducens nerve, controls the outside pulling muscle, or lateral rectus. If this nerve is damaged, the outside pulling muscle is paralyzed, and large angle eye crossing of one eye results. Causes of nerve damage can be increased intracranial pressure, viral syndrome or tumor. This condition requires an MRI scan to determine the cause. Treatments include addressing the root cause of the problem and possible eye muscle surgery.

Duane’s syndrome is the congenital absence of the sixth nerve or abducens nerve. It causes decreased eye movements in the outward direction of one eye. Many children with this condition will develop a head turn to move the normal eye into alignment with the abnormal eye. Unlike a 6th nerve palsy, this condition is rarely associated with other neurological problems. Neuroimaging (MRI) is generally not needed. Duane’s syndrome can be treated with glasses, patching or eye muscle surgery.

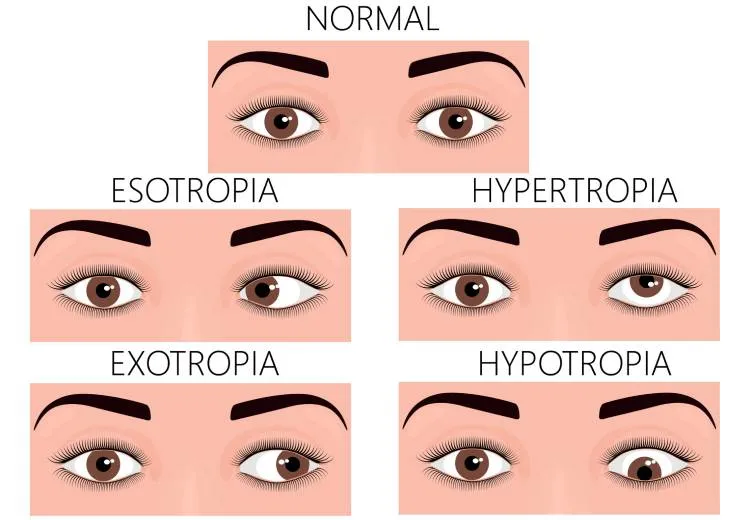
Vertical strabismus is when the eyes are offset vertically, or one eye is higher or lower than the other. It can be caused by a 4th nerve palsy (superior oblique muscle palsy), damage to one of the vertical muscles, or thyroid eye disease. It can be treated with prism eyeglasses, or eye muscle surgery to relieve double vision.
Pseudostrabismus is the false appearance of eye misalignment caused by the shape of the eyelids. Many children can have prominent eyelid folds that allow you to see more of the white part of the eye on the outside corner rather than the inside corner. When the child looks to the side, the eye moving in gets buried under the eyelid making it appear to move in further than the other eye. This is not true eye misalignment, and no treatment is needed. This appearance generally gets better with growth of the face and eyelids. It is important to see Dr. Morrison for a full evaluation for this condition. If true strabismus is not diagnoses and treated, permanent vision loss could result.

This is an outpatient surgery that takes about 45 minutes to complete. A small incision is made on the white part of the eye to access the muscle. The muscle is physically moved on the eye to make it weaker or stronger. There are no patches or bandages after surgery, although the eye is red at the incision site. Dr. Morrison has successfully completed over 6,000 eye muscle surgeries in his career.
